Our story is similar to many others we have seen... is it similar to yours?
Update 09/02/2022 - Just in time for Mom's birthday, we received the amended death certificate showing the immediate cause of death was multi-organ failure due to multi-drug toxicity and adverse drug reactions.

We can’t help but be upset Mom went to the hospital for oxygen and expected to be released, and never came home after they gave her Remdesivir. As Mom's oldest Son, and Medical Power of Attorney - I had a responsibility and Love for our Mom - my Wife's best friend and confidant of 30 years.
Mom had been feeling nauseous for a few days - starting on Wednesday November 10, 2021. She monitored her vitals and thought it was a short term thing. Over the weekend she wasn't feeling any better, and Monday she wanted to get checked. We went to the nearest clinic - no walk-ins due to 'COVID'. We went to her primary care physician - no walk-ins and directed us to their nearest walk-in clinic. By this time she low oxygen saturation and was getting weak - we had been doing this for over an hour. A clinic staff met us outside with a wheelchair - and would not let her in without a mask; she was visibly struggling for air and strength. After a bit of a firm challenge - were they really going to turn away a person who was visibly in respiratory distress - they brought us to a room. The medical assist asked routine questions, took vitals, and put Mom on oxygen - she went from mid 60s O2 saturation to low 90s and immediately began improving. Then the doctor came in.
Initial exam was a cough and low oxygen saturation - nothing else, and she said Mom was not symptomatic for 'COVID' - and they would do a quick 15-minute PCR test as standard protocol. This is the same PCR test the CDC in June 2021 had advised be discontinued by 12/31/2021 due to the high false-positives, and the extended false-positives up to 12 weeks post-exposure to 'COVID'. In less than five minutes the doctor came back upset - advising she was 'COVID' positive, she had every "hidden" symptom, and we had potentially infected the entire clinic. After a brief firm reminder this was not the time for lectures, she told Mom she was calling an ambulance to take her to the emergency room.
Mom didn’t want to go to the hospital - we had long had these discussions – I didn’t want her to go – and they told her if she didn’t she would die. She asked to be sent home with oxygen or a prescription for me to pick up an O2 machine - they could not send her home with oxygen… only the hospital could. Then the doctor told Mom she could go home - and she would die. Nothing else, and very cold - the doctor was still very mad because we refused to wear masks. She had the right to refuse, and when the paramedics arrived they all said she would go for oxygen and most are released home - she was no longer in any distress and would likely go home. Mom very reluctantly went. By mid-afternoon we had conversations with attending physicians and Mom was greatly improved. We waited to be called to pick her up. I simply should have - I didn't. We were able to monitor her medical chart and progress online. Her x-rays were mostly clear - no indications of 'COVID' or pneumonia. Her labs showed elevated bacteria - about 330s. The attending physician called and said they would keep her overnight for observation and she was doing well, improving. As we continued to monitor, and talk to Mom, she sounded better and was ready to be home the next day. She was then taken to the COVID floor and given two initial doses of Remdesivir right away. She never signed a hospital treatment / billing consent form; instead – in the signature space someone had written “COVID” across it. Remdesivir is the only FDA approved protocol for COVID positive treatment. As part of the EUA and then approval, there are three specific criteria in advising patients: 1) consent; 2) side effects warning, and 3) it is the only protocol and was not developed for COVID. Mom was given none of these.
As her Next-of-Kin and Medical Power of Attorney, I was called the next day and advised of the use of Remdesivir. I asked about Ivermectin and/or Hydroxychloroquine – and was told there was no protocol for Ivermectin and/or Hydroxychloroquine use and none available in the hospital – only Remdesivir. Our Mom died five days later – and I was repeatedly told she had to improve in five days, or her chances were she would not leave the hospital. I never understood why this was repeated, until my Wife researched Remdesivir the same as she had researched other protocols, including Ivermectin and/or Hydroxychloroquine.
On Tuesday we checked her blood work online and found the bacteria was down to below 30 and in the normal range. We thought for sure Mom would be coming home. Mom continued to sound good, and thought she would be coming home. The new attending physician said they needed to treat her for the 'COVID' she had tested positive for. I asked if they were going to use Ivermectin or Hydroxychloroquine - no, their protocol was Remdesivir - nothing else was explained (as we later learned is required by the FDA Emergency Use Authorization). I had confused Remdesivir with something else, and will forever regret this. My Wife was concerned. It was too late - we also did not know they started the protocol at her admission the day before - two doses ($5,000).
On Wednesday her medical chart showed 'COVID Pneumonia' and specifically bacterial pneumonia ('COVID' is viral, not bacterial; and there is both viral and bacterial pneumonia). Her x-rays also showed pneumonia and/or 'COVID'. To this time I had been denied going up - because I would not wear a mask, and we also thought Mom would be coming home.
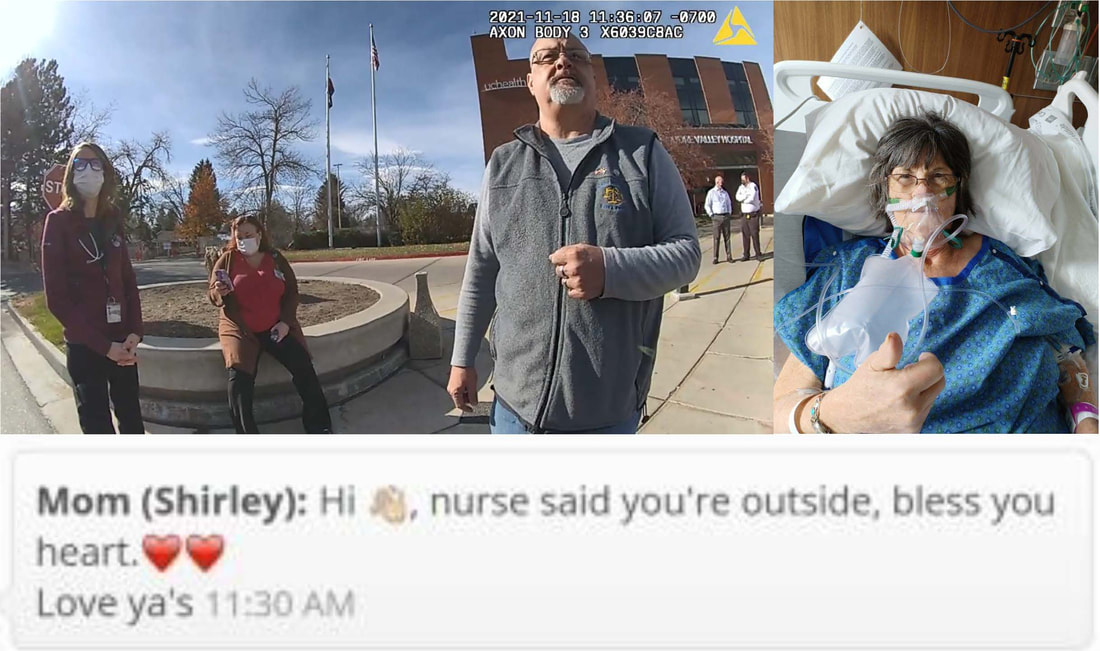
On Thursday morning I woke up to the realization - and fear - Mom would not be leaving the hospital. I had never been so upset in my life. I told my Wife I was going to the hospital and either seeing Mom or if I could bring her to our home - of course, and she made the room Mom would stay in ready for her. On my way the hospital family care team called - and they only call for one reason. They explained Mom was declining, and if she could make it through the weekend - five days - her chances of recovery were better, and they were concerned about her decline and the weekend (turns out Remdesivir has a 30% fatality rate in the first five days). We agreed to meet outside and make a plan, and I was firm I would be seeing our Mom that day. When I arrived, I called and waited. A team of staff - three females and two male security guards (who I had previously had less than positive interactions with two weeks prior - when dad was at the ER). The antagonistic security supervisor kept getting closer trying to intimidate me (as he did two weeks prior). In an emotional and grieving state, I did not want to be antagonized and directed him to step away from me. He would not, and he would not let me privately talk to the staff. I called the police. In reviewing the bodycam videos, he made it very clear the plan was to call the police themselves, and I beat them to it. As I spoke to the care team and supervisors, I told them we needed a visitation plan - patients having visitors was the best path to recovery; and denying visitors was a path to decline. I was told - its been a moral dilemma they have faced (turns out - this exact statement has been told to other families with similar stories). I reminded them it is not a moral dilemma - it is immoral and unethical to knowingly allow a patient to die without their best efforts - and if our Mom died, it was on them. The reason for denying visitation was now because I had been exposed to 'COVID' taking Mom to clinics, and needed to wait 10 days. I had just been told she may not make it through the weekend, I reminded them of this. I then decided - and stated - it would be best for me to exercise my Medical Power of Attorney and take her home. Mom may die on the way, or at home - and at least she would be with loved ones. I was then assured they would find a solution for me to visit - at least before the weekend. I then had a video call with Mom that afternoon, and she looked and sounded pretty good. I had also again - as I did before - asked about Ivermectin or Hydroxychloroquine - again no, their only protocol was Remdesivir.
On Friday it was planned to have another video call. Our youngest daughter lives in the area and Fridays are early days. She offered to get our twin grandsons early from school and have a picnic at the hospital for the video call. They are excellent artists and drew their GG some nice pictures, and I got some photos from her house to put near her, and a card from all of us - and a note of love and encouragement. The video call went well and we had hopes; however, our hopes were not as high. Unfortunately, overnight Mom further declined and she was on a BPAP machine with a full mask - she could not see her phone to text, or use it to call. After going to Mom's house, about 5:30pm, I was called by the hospital supervisor telling me they created a visitation policy exception for me - as approved by the hospital system corporate and CDC. Essentially, I needed to be tested and if negative could go up for an hour each day; if I was positive it would only be for end of life conversations. I asked for this in writing. About 15 minutes later I received an email with the written policy. However, in the written policy it stated if I was positive there would be no visitation for any reason. I called the hospital supervisor and was told she did not change anything, it was as we discussed - I let her know it was recorded and exactly what she said. She had no answer, other than if I wanted to visit, I had to be negative. I scheduled the first available testing at one of their clinics (required) for Saturday at 9:00am.
On Saturday I was called at 7:00am by the attending physician, a new one. She asked what my plan was for the day and I told her. She then told me to not get tested and to come straight up to Mom's room - she would not make it through the weekend. She explained, under the policy given - if I was positive she would not be able to allow me up, and she couldn't take that chance - she couldn't let Mom die alone. She was the only hospital staff to say this. She told me she would let security know. I got to the hospital at 7:19am and was wearing a mask, as required. Hospital security tried to stop me, I didn't slow down. They yelled I needed 'COVID' screened - like I would take that chance. I heard one security guard on his radio say, "The subject is in the building. He is wearing a mask, but did not stop for screening." By the time I was at the elevator, I could hear him again, "The subject is at the elevators - someone needs to stop him before he gets to the 4th floor." I was prepared for it to get interesting. It didn't. I was directed to the Charge Nurse and attending physician, I gowned up and told I could stay as long as I wanted - they were concerned if I left for any reason, I would not be allowed back up.
I hustled in the room and immediately took my mask off so Mom could see me* (*there are cameras in patient rooms - I was immediately told if I took my mask off again, I would have to leave and not allowed to return). She was so surprised and happy - "I thought they wouldn't let you up!" - "You know me Mom, nothing will keep me away." I told her why I was there - to help her make it through the weekend - and she said - "Yes, I'm going home." and I told her Karen made up her room at our house for her to stay as long as she needed and wanted. I made sure Mom talked to everyone on the phone. Mom slowly declined - starting about 10:45am, and more so starting about 2:15pm. I held her for twelve hours. She died, so she would no longer suffer, at 7:00pm. I escorted her down to the hospital morgue and said goodbye.
Remdesivir has a long history – and not a good one. When it was first developed and used for Ebola, it had about a 50% fatality rate and was pulled worldwide. It was forgotten about until the events of 2020. The FDA very quickly gave an EUA – and would not approve others, even for studies, because, “There is insufficient evidence of its efficacy or potential harm to approve or deny; and is therefore denied EUA.” This left ONLY Remdesivir. Since its EUA and then approval as the only protocol – CDC has reported, indirectly, the fatality rate of Remdesivir as 1 in 3 within five days. Patients do not die of COVID – they die of multi-organ system failure. But, that’s not on the death certificate – it is in their blood work.
In January my dad was taken to the same ER after symptoms and tested COVID positive. He lives alone and had no one with him for over a week prior – we went to Indiana for the death of my Wife’s mom. There was no possibility of exposure or transmission for him. He was examined and released to medical rehab on antibiotics (for bacterial pneumonia – COVID is a viral infection; Mom also had bacterial pneumonia) and oxygen. He was admitted a second time – and as his MPOA, I told them they could not use Remdesivir. They actually argued with me and said they would not take medical directives from a lay person. I reminded them his MPOA specifically authorized me to do exactly that. They looked at his MPOA on file and then told me they no longer use Remdesivir in the protocol. There is no longer a COVID protocol at this hospital (or their entire system in Colorado).
Why are hospitals administering a drug with a 1 in 3 fatality rate; and no other protocol – including the proven Ivermectin and/or Hydroxychloroquine? If you look at the FDA approval and prior EAU, under the CARES Act and Americans Recovery Act, hospitals are given a 20% compensation on the ENTIRE hospital bill if – and this is the criteria – they administer Remdesivir. Remdesivir is $2,500 per dose (five days – six doses - $15K for every patient – dead or alive) and the Ivermectin and/or Hydroxychloroquine protocols – less than $15 per dose / a day. What are the side-effects of the Ivermectin and/or Hydroxychloroquine protocols? Some typical minor issues – diarrhea, nausea, chills, general discomfort. Nothing serious – as seen with Remdesivir – multi-organ system failure and death have never been recorded with Ivermectin and/or Hydroxychloroquine protocols. There is simply no reason to not authorize Ivermectin and/or Hydroxychloroquine.
Hospitals are given $13,000 for each COVID admission, and even more for each COVID death. Mom’s $80K hospital bill was worth another $50K – her death was worth $50K in taxpayer monies and 100% profit to the hospital. Death is difficult. This is unconscionable. Hundreds of thousands of lives could have been saved. Not just one – hundreds of thousands. Ivermectin and/or Hydroxychloroquine are preventive and active treatments. Remdesivir should, again, be banned.
Mom had been feeling nauseous for a few days - starting on Wednesday November 10, 2021. She monitored her vitals and thought it was a short term thing. Over the weekend she wasn't feeling any better, and Monday she wanted to get checked. We went to the nearest clinic - no walk-ins due to 'COVID'. We went to her primary care physician - no walk-ins and directed us to their nearest walk-in clinic. By this time she low oxygen saturation and was getting weak - we had been doing this for over an hour. A clinic staff met us outside with a wheelchair - and would not let her in without a mask; she was visibly struggling for air and strength. After a bit of a firm challenge - were they really going to turn away a person who was visibly in respiratory distress - they brought us to a room. The medical assist asked routine questions, took vitals, and put Mom on oxygen - she went from mid 60s O2 saturation to low 90s and immediately began improving. Then the doctor came in.
Initial exam was a cough and low oxygen saturation - nothing else, and she said Mom was not symptomatic for 'COVID' - and they would do a quick 15-minute PCR test as standard protocol. This is the same PCR test the CDC in June 2021 had advised be discontinued by 12/31/2021 due to the high false-positives, and the extended false-positives up to 12 weeks post-exposure to 'COVID'. In less than five minutes the doctor came back upset - advising she was 'COVID' positive, she had every "hidden" symptom, and we had potentially infected the entire clinic. After a brief firm reminder this was not the time for lectures, she told Mom she was calling an ambulance to take her to the emergency room.
Mom didn’t want to go to the hospital - we had long had these discussions – I didn’t want her to go – and they told her if she didn’t she would die. She asked to be sent home with oxygen or a prescription for me to pick up an O2 machine - they could not send her home with oxygen… only the hospital could. Then the doctor told Mom she could go home - and she would die. Nothing else, and very cold - the doctor was still very mad because we refused to wear masks. She had the right to refuse, and when the paramedics arrived they all said she would go for oxygen and most are released home - she was no longer in any distress and would likely go home. Mom very reluctantly went. By mid-afternoon we had conversations with attending physicians and Mom was greatly improved. We waited to be called to pick her up. I simply should have - I didn't. We were able to monitor her medical chart and progress online. Her x-rays were mostly clear - no indications of 'COVID' or pneumonia. Her labs showed elevated bacteria - about 330s. The attending physician called and said they would keep her overnight for observation and she was doing well, improving. As we continued to monitor, and talk to Mom, she sounded better and was ready to be home the next day. She was then taken to the COVID floor and given two initial doses of Remdesivir right away. She never signed a hospital treatment / billing consent form; instead – in the signature space someone had written “COVID” across it. Remdesivir is the only FDA approved protocol for COVID positive treatment. As part of the EUA and then approval, there are three specific criteria in advising patients: 1) consent; 2) side effects warning, and 3) it is the only protocol and was not developed for COVID. Mom was given none of these.
As her Next-of-Kin and Medical Power of Attorney, I was called the next day and advised of the use of Remdesivir. I asked about Ivermectin and/or Hydroxychloroquine – and was told there was no protocol for Ivermectin and/or Hydroxychloroquine use and none available in the hospital – only Remdesivir. Our Mom died five days later – and I was repeatedly told she had to improve in five days, or her chances were she would not leave the hospital. I never understood why this was repeated, until my Wife researched Remdesivir the same as she had researched other protocols, including Ivermectin and/or Hydroxychloroquine.
On Tuesday we checked her blood work online and found the bacteria was down to below 30 and in the normal range. We thought for sure Mom would be coming home. Mom continued to sound good, and thought she would be coming home. The new attending physician said they needed to treat her for the 'COVID' she had tested positive for. I asked if they were going to use Ivermectin or Hydroxychloroquine - no, their protocol was Remdesivir - nothing else was explained (as we later learned is required by the FDA Emergency Use Authorization). I had confused Remdesivir with something else, and will forever regret this. My Wife was concerned. It was too late - we also did not know they started the protocol at her admission the day before - two doses ($5,000).
On Wednesday her medical chart showed 'COVID Pneumonia' and specifically bacterial pneumonia ('COVID' is viral, not bacterial; and there is both viral and bacterial pneumonia). Her x-rays also showed pneumonia and/or 'COVID'. To this time I had been denied going up - because I would not wear a mask, and we also thought Mom would be coming home.
On Thursday morning I woke up to the realization - and fear - Mom would not be leaving the hospital. I had never been so upset in my life. I told my Wife I was going to the hospital and either seeing Mom or if I could bring her to our home - of course, and she made the room Mom would stay in ready for her. On my way the hospital family care team called - and they only call for one reason. They explained Mom was declining, and if she could make it through the weekend - five days - her chances of recovery were better, and they were concerned about her decline and the weekend (turns out Remdesivir has a 30% fatality rate in the first five days). We agreed to meet outside and make a plan, and I was firm I would be seeing our Mom that day. When I arrived, I called and waited. A team of staff - three females and two male security guards (who I had previously had less than positive interactions with two weeks prior - when dad was at the ER). The antagonistic security supervisor kept getting closer trying to intimidate me (as he did two weeks prior). In an emotional and grieving state, I did not want to be antagonized and directed him to step away from me. He would not, and he would not let me privately talk to the staff. I called the police. In reviewing the bodycam videos, he made it very clear the plan was to call the police themselves, and I beat them to it. As I spoke to the care team and supervisors, I told them we needed a visitation plan - patients having visitors was the best path to recovery; and denying visitors was a path to decline. I was told - its been a moral dilemma they have faced (turns out - this exact statement has been told to other families with similar stories). I reminded them it is not a moral dilemma - it is immoral and unethical to knowingly allow a patient to die without their best efforts - and if our Mom died, it was on them. The reason for denying visitation was now because I had been exposed to 'COVID' taking Mom to clinics, and needed to wait 10 days. I had just been told she may not make it through the weekend, I reminded them of this. I then decided - and stated - it would be best for me to exercise my Medical Power of Attorney and take her home. Mom may die on the way, or at home - and at least she would be with loved ones. I was then assured they would find a solution for me to visit - at least before the weekend. I then had a video call with Mom that afternoon, and she looked and sounded pretty good. I had also again - as I did before - asked about Ivermectin or Hydroxychloroquine - again no, their only protocol was Remdesivir.
On Friday it was planned to have another video call. Our youngest daughter lives in the area and Fridays are early days. She offered to get our twin grandsons early from school and have a picnic at the hospital for the video call. They are excellent artists and drew their GG some nice pictures, and I got some photos from her house to put near her, and a card from all of us - and a note of love and encouragement. The video call went well and we had hopes; however, our hopes were not as high. Unfortunately, overnight Mom further declined and she was on a BPAP machine with a full mask - she could not see her phone to text, or use it to call. After going to Mom's house, about 5:30pm, I was called by the hospital supervisor telling me they created a visitation policy exception for me - as approved by the hospital system corporate and CDC. Essentially, I needed to be tested and if negative could go up for an hour each day; if I was positive it would only be for end of life conversations. I asked for this in writing. About 15 minutes later I received an email with the written policy. However, in the written policy it stated if I was positive there would be no visitation for any reason. I called the hospital supervisor and was told she did not change anything, it was as we discussed - I let her know it was recorded and exactly what she said. She had no answer, other than if I wanted to visit, I had to be negative. I scheduled the first available testing at one of their clinics (required) for Saturday at 9:00am.
On Saturday I was called at 7:00am by the attending physician, a new one. She asked what my plan was for the day and I told her. She then told me to not get tested and to come straight up to Mom's room - she would not make it through the weekend. She explained, under the policy given - if I was positive she would not be able to allow me up, and she couldn't take that chance - she couldn't let Mom die alone. She was the only hospital staff to say this. She told me she would let security know. I got to the hospital at 7:19am and was wearing a mask, as required. Hospital security tried to stop me, I didn't slow down. They yelled I needed 'COVID' screened - like I would take that chance. I heard one security guard on his radio say, "The subject is in the building. He is wearing a mask, but did not stop for screening." By the time I was at the elevator, I could hear him again, "The subject is at the elevators - someone needs to stop him before he gets to the 4th floor." I was prepared for it to get interesting. It didn't. I was directed to the Charge Nurse and attending physician, I gowned up and told I could stay as long as I wanted - they were concerned if I left for any reason, I would not be allowed back up.
I hustled in the room and immediately took my mask off so Mom could see me* (*there are cameras in patient rooms - I was immediately told if I took my mask off again, I would have to leave and not allowed to return). She was so surprised and happy - "I thought they wouldn't let you up!" - "You know me Mom, nothing will keep me away." I told her why I was there - to help her make it through the weekend - and she said - "Yes, I'm going home." and I told her Karen made up her room at our house for her to stay as long as she needed and wanted. I made sure Mom talked to everyone on the phone. Mom slowly declined - starting about 10:45am, and more so starting about 2:15pm. I held her for twelve hours. She died, so she would no longer suffer, at 7:00pm. I escorted her down to the hospital morgue and said goodbye.
Remdesivir has a long history – and not a good one. When it was first developed and used for Ebola, it had about a 50% fatality rate and was pulled worldwide. It was forgotten about until the events of 2020. The FDA very quickly gave an EUA – and would not approve others, even for studies, because, “There is insufficient evidence of its efficacy or potential harm to approve or deny; and is therefore denied EUA.” This left ONLY Remdesivir. Since its EUA and then approval as the only protocol – CDC has reported, indirectly, the fatality rate of Remdesivir as 1 in 3 within five days. Patients do not die of COVID – they die of multi-organ system failure. But, that’s not on the death certificate – it is in their blood work.
In January my dad was taken to the same ER after symptoms and tested COVID positive. He lives alone and had no one with him for over a week prior – we went to Indiana for the death of my Wife’s mom. There was no possibility of exposure or transmission for him. He was examined and released to medical rehab on antibiotics (for bacterial pneumonia – COVID is a viral infection; Mom also had bacterial pneumonia) and oxygen. He was admitted a second time – and as his MPOA, I told them they could not use Remdesivir. They actually argued with me and said they would not take medical directives from a lay person. I reminded them his MPOA specifically authorized me to do exactly that. They looked at his MPOA on file and then told me they no longer use Remdesivir in the protocol. There is no longer a COVID protocol at this hospital (or their entire system in Colorado).
Why are hospitals administering a drug with a 1 in 3 fatality rate; and no other protocol – including the proven Ivermectin and/or Hydroxychloroquine? If you look at the FDA approval and prior EAU, under the CARES Act and Americans Recovery Act, hospitals are given a 20% compensation on the ENTIRE hospital bill if – and this is the criteria – they administer Remdesivir. Remdesivir is $2,500 per dose (five days – six doses - $15K for every patient – dead or alive) and the Ivermectin and/or Hydroxychloroquine protocols – less than $15 per dose / a day. What are the side-effects of the Ivermectin and/or Hydroxychloroquine protocols? Some typical minor issues – diarrhea, nausea, chills, general discomfort. Nothing serious – as seen with Remdesivir – multi-organ system failure and death have never been recorded with Ivermectin and/or Hydroxychloroquine protocols. There is simply no reason to not authorize Ivermectin and/or Hydroxychloroquine.
Hospitals are given $13,000 for each COVID admission, and even more for each COVID death. Mom’s $80K hospital bill was worth another $50K – her death was worth $50K in taxpayer monies and 100% profit to the hospital. Death is difficult. This is unconscionable. Hundreds of thousands of lives could have been saved. Not just one – hundreds of thousands. Ivermectin and/or Hydroxychloroquine are preventive and active treatments. Remdesivir should, again, be banned.
Mom’s bill was about $80K – which insurance denied all but about $4,000 (I don’t know if this is because they admitted her as unvaccinated, noted on her chart – and the admitting financial responsibility form has 'COVID' written where she was to sign; in another 'COVID' admission, the person wasn’t noted as unvaccinated and all the bills were paid for).
Hospitals are reimbursed under the CARES Act and Americans Recovery Act, and a few others – and get an extra 20% compensation of the full bill for administering Remdesivir (for Mom - an extra $16K), then $13K for a COVID positive admission, and $39K for a COVID positive death ($68K extra above the bill) – and they will be reimbursed for any amount insurance denied under the various recovery acts; almost $150K for Mom’s death. Hospitals are profiting quite well (Remdesivir is $2,500 each – gave her two after admission, then one each day Tue-Fri).
This is evil – and they have been killing our loved ones.
These protocols have killed tens of thousands nationwide as we write this. There are a series of bills in Colorado's legislature - 1) required visitation during a pandemic; and 2) the right to choose medications - including Ivermectin and Hydroxychloroquine (this one has died - "postponed indefinitely" in the first committee, without any hearing or testimony).
Hospitals are reimbursed under the CARES Act and Americans Recovery Act, and a few others – and get an extra 20% compensation of the full bill for administering Remdesivir (for Mom - an extra $16K), then $13K for a COVID positive admission, and $39K for a COVID positive death ($68K extra above the bill) – and they will be reimbursed for any amount insurance denied under the various recovery acts; almost $150K for Mom’s death. Hospitals are profiting quite well (Remdesivir is $2,500 each – gave her two after admission, then one each day Tue-Fri).
This is evil – and they have been killing our loved ones.
These protocols have killed tens of thousands nationwide as we write this. There are a series of bills in Colorado's legislature - 1) required visitation during a pandemic; and 2) the right to choose medications - including Ivermectin and Hydroxychloroquine (this one has died - "postponed indefinitely" in the first committee, without any hearing or testimony).